New alliance calls on province to increase access to treatment for opioid addiction
A new alliance of health-care workers, researchers and those with lived experience will launch at Queen’s Park on Friday.
The group is recommending the province make policy changes to break down barriers people face when accessing treatment for opioid addiction.
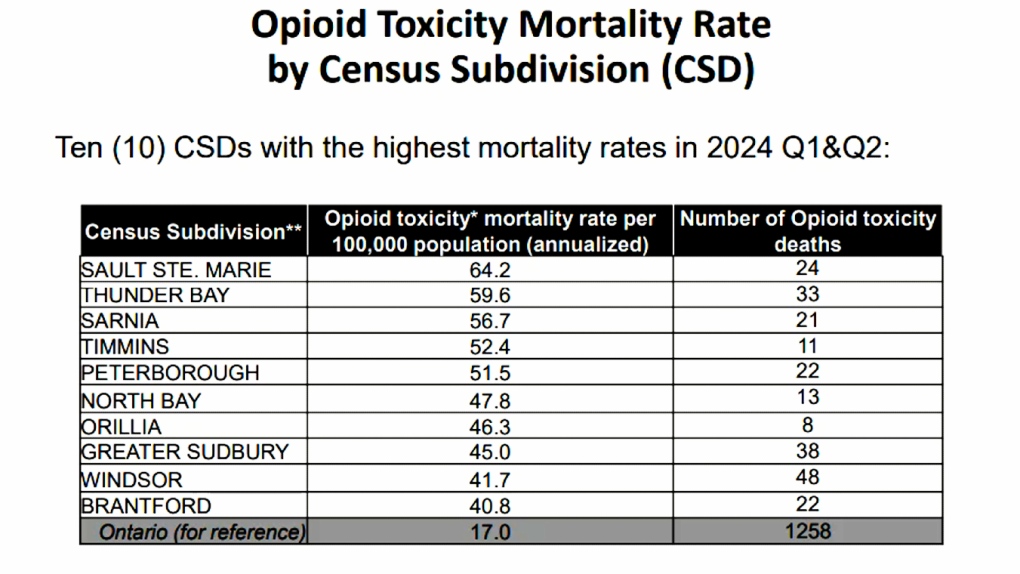 The number of opioid toxicity deaths in the four major northern cities ranges from 38 in Sudbury to 24 in Sault Ste. Marie, 13 in North Bay and 11 in Timmins. (Lydia Chubak/CTV News)
The number of opioid toxicity deaths in the four major northern cities ranges from 38 in Sudbury to 24 in Sault Ste. Marie, 13 in North Bay and 11 in Timmins. (Lydia Chubak/CTV News)
Seamus Murphy of Timmins is part of One Step Forward, a group working to help people get barrier-free access to treatment for opioid addiction. He's also deputy chief for Cochrane District Paramedic Service in Timmins.
Murphy’s desire to help is twofold. He’s a paramedic and two years ago, he lost a niece to an opioid overdose.
"You know, I thought people chose to use drugs. And the data shows that over 70 per cent were prescribed at first with opiates," said Murphy, a member of the Cochrane District Paramedic Service.
"That is because opiates are prescribed for pain and it can be any kind of pain. And that's what happened with my niece. So, you know, we have to try to work together across the district and across the agencies so that we can get, you know, at least a few positive outcomes doing this."
The alliance is rallying at Queen’s Park, asking the province for policy changes to help combat Ontario’s opioid crisis.
 One Step Forward, a new alliance, is bringing its four main recommendations to increase access for opioid addiction treatment to Queen’s Park on Friday. (Lydia Chubak/CTV News Northern Ontario)
One Step Forward, a new alliance, is bringing its four main recommendations to increase access for opioid addiction treatment to Queen’s Park on Friday. (Lydia Chubak/CTV News Northern Ontario)
The alliance has four main recommendations for the province: establish a cross-ministry emergency task force; launch and fund a virtual opioid addiction treatment service; ensure a patient-centred approach; and, empower pharmacists to play a greater role.
Researchers with the alliance said they discovered that in the past four years, despite an increase in opioid addiction, there’s been no increase in the number of Ontarians being treated for opioid use disorder.
"We did find, in fact, that there were a lot of barriers to access to treatment," said Jason Grier of Delphic Research.
"The most sort of common treatment pathway, you know, it really didn't represent a good option (for) all people."
Individual recovery needs
Grier said people dealing with addiction have their own set of circumstances, but the system isn’t responding to their needs.
"The recovery journey needs to be as individual as they are," he said.
"And so that fundamentally, that was the barrier."
The province’s chief coroner’s office recently released opioid toxicity rates and all major northern Ontario cities rank in the Top 10 for the highest mortality rates in the first half of 2024.
The number of opioid toxicity deaths in the four major northern cities ranges from 38 in Sudbury to 24 in Sault Ste. Marie, 13 in North Bay and 11 in Timmins.
Murphy said since 2017, 196 people in the Cochrane district have died from an opioid overdose. Only four were homeless and he said 95 per cent of the deaths happened in Timmins.
Grier said it doesn't need to be that way.
"With the right treatment and the right support in a stigma-free setting, people can recover," he said.
"I've met people who have gone on that journey. And I think that is very heartening. I think that is something I hope all of us would take to heart, that we can do better and we can help people on this journey to recovery and they can go on to lead better lives."
- Download the CTV News app now
- Get local breaking news alerts
- Daily newsletter with the top local stories emailed to your inbox
Murphy said paramedics with Cochrane District Paramedic Service are equipped to offer treatments to prevent overdoses and said more people are accepting suboxone and buprenorphine/naloxone.
"Last Friday, we had a patient that was treated by us with buprenorphine/naloxone (and) brought to the hospital," he said.
"He then refused treatment because he felt great. So he left. Next day he realized that, hey, I actually feel good on treatment. So he went in and he's now put into long-term treatment. So these are wins for us."
There can be more success stories, he said, if people are offered treatment that works for them.
CTVNews.ca Top Stories

Trudeau's 2024: Did the PM become less popular this year?
Justin Trudeau’s numbers have been relatively steady this calendar year, but they've also been at their worst, according to tracking data from CTV News pollster Nik Nanos.
Manhunt underway after woman, 23, allegedly kidnapped, found alive in river
A woman in her 20s who was possibly abducted by her ex is in hospital after the car she was in plunged into the Richelieu River.
Calling all bloodhounds: These P.E.I. blood donors have four legs and a tail
Dogs are donating blood and saving the lives of canines at the University of Prince Edward Island's Atlantic Veterinary College in Charlottetown.
Summer McIntosh makes guest appearance in 'The Nutcracker'
Summer McIntosh made a splash during her guest appearance in The National Ballet of Canada’s production of 'The Nutcracker.'
A 9-year-old is among 5 killed in the Christmas market attack in Germany
A nine-year-old was among five people killed when a Saudi doctor intentionally drove into a Christmas market teeming with holiday shoppers in the German city of Magdeburg, an official said Saturday.
Wild boar hybrid identified near Fort Macleod, Alta.
Acting on information, an investigation by the Municipal District of Willow Creek's Agricultural Services Board (ASB) found a small population of wild boar hybrids being farmed near Fort Macleod.
Toronto firefighters rescue man who fell into sinkhole in Yorkville
A man who fell into a sinkhole in Yorkville on a snowy Friday night in Toronto has been rescued after being stuck in the ground for roughly half an hour.
Winning $20-million Lotto Max ticket sold in Hamilton
Someone who purchased a Lotto Max ticket in Hamilton for Friday night’s draw is now $20-million richer.
Overheated immigration system needed 'discipline' infusion: minister
An 'overheated' immigration system that admitted record numbers of newcomers to the country has harmed Canada's decades-old consensus on the benefits of immigration, Immigration Minister Marc Miller said, as he reflected on the changes in his department in a year-end interview.