Sudbury, Ont., doctor says LTC care homes becoming a ‘dumping ground’ for psychiatric patients
Ontario’s long-term care homes are feeling the effects of hospital overcrowding, a Sudbury doctor says, with severely ill and psychiatric patients being moved to LTC to free up hospital beds.
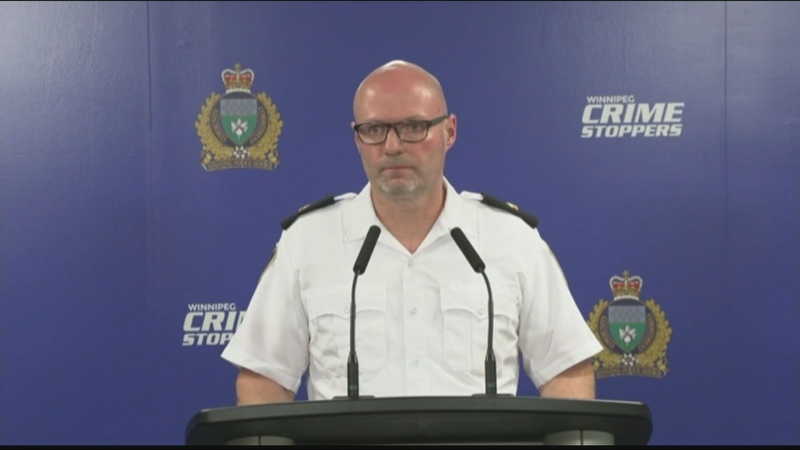
Dr. Maurice St. Martin is a Sudbury physician with four decades of experience in long-term care. He is a medical director at Pioneer Manor and, more recently, the attending physician and medical director at St. Joseph’s Villa.
St. Martin said one of his main concerns is inappropriate admissions to long-term-care homes.
“We’re making the situation worse in these facilities by throwing in residents that are not appropriate,” he said.
St. Martin said more patients with severe mental health needs are arriving at long-term care homes, which staff are not equipped to handle.
“We are becoming a dumping ground, literally, for psychiatric patients,” St. Martin said.
Not only is LTC not the right setting for them, the traditional life expectancy of a long-term-care resident is two-and-a-half to three years.
“When you admit a 50-year-old schizophrenic, who might be better suited for a March of Dimes assisted living home or other type of setting, they pose a real threat to your 80, 90-year-old demented patients,” he said.
St. Martin adds that this also leads to a bed shortage.
“If you’re expecting a life expectancy of three years, that person lives to 80 years of age, 10 residents could have used that one bed,” he said.
“So that’s a prime example of bed blocking within the system. We’re creating our own roadblocks within the system.”
St. Martin said the pandemic has exposed some of the other issues in long-term care homes.
“I’ve put my soul into taking care of the frail, elderly population,” St. Martin said.
“I’ve come to realize long-term care is the Achilles heel of the health care system. We’ve all seen that with COVID and unfortunately, despite the fact we’ve worked through all this mess, it seems to be getting worse in the last few months.”
St. Martin said the primary issue is a lack of communication and transparency between community partners, like hospitals and Home and Community Care Support Services (HCCSS).
“There’s been instances where community partners have literally lied about the status of these residents to get them admitted into institutions,” he said.
St. Martin gave the example of a 95-year-old woman that was to be admitted into one of his LTC homes who fractured her neck. He said the fracture was inoperable, but after calling the hospital, St. Martin was told she was cleared to be admitted into the LTC care facility.
The Ministry of Long-term Care, which administers Ontario’s long-term care system, said in a statement that a patient is discharged from hospital when their doctor determines they no longer require urgent care.
“Patients (then) begin to work with a (HCCSS) coordinator to determine proper placement and that prospective long-term care home can meet the resident's care needs,” the statement said.
“Long-term care homes will also not approve an applicant’s admission to a home if their staff lacks the nursing expertise necessary to meet the applicant’s care requirements.”
That may be the policy, but St. Martin said that hasn’t been his experience.
'THE PERSON WAS IN DELIRIUM'
“The person was in delirium in the hospital and had to be restrained,” he said.
“That (level of care is) not available in long-term care. Our community partners know that.”
CTV News reached out to Home and Community Care Support Services for an interview to inquire about individuals being placed in LTC, which may not be the best setting for them.
We received a statement that said, in part:
“Home and Community Care Support Services works closely with patients to complete assessments and determine eligibility for long-term care home placement … Any patient, family or caregiver with concerns about their current placement or care are encouraged to reach out to their care coordinator who will work with them to address their concerns.”
St. Martin said there has also been an increase in palliative care patients, who he said would be better placed in hospice facilities.
“In the last six months, two HSN admissions were made palliative on the day of admission,” he said.
“Those patients were imminently dying.”
Salah Shadir from the Ontario Health Coalition said that these types of cases are being seen across the province, not just in Sudbury.
Shadir points to staffing shortages across all aspects of health care as the root cause.
“In long-term care, there are long wait lists, but as well, when you look at home care, when you look at palliative care, hospice care, everything is full,” Shadir said.
He said there is a waitlist of 30,000 people looking to access long-term care, something that leads to individuals ending up in long-term care when it might not be the best place for them.
“What we’re seeing is people who have mental health behaviour issues, but that’s a completely different situation and that requires higher staffing levels than what we currently have in long term care,” Shadir said.
NOT EQUIPPED TO CARE FOR THEM
“Long-term care is not built or equipped with enough staffing to deal with the increased acuity and the increased level of care for those kind of patients.”
In a statement to CTV News, a spokesperson for Health Sciences North said the decision where to send people when they are discharged from hospital is a collaborative process.
It involves “comprehensive assessments among hospital staff, the patient’s health care providers and support services, such as Home and Community Care Support Services, and including the patient, family and/or caregiver(s).”
“The coordination of patient placement in long-term care, including eligibility and suitability of long term care homes, is determined by Home and Community Care Support Services Placement Coordinators and not by HSN staff or physicians,” the statement said.
Additionally, St. Martin said there have been numerous occasions where patient information has been outdated by six months.
“In six months, a lot can happen with these frail elderly, from heart attacks, falling, strokes,” he said. “That information needs to be known so that we can provide proper care.”
Despite the challenges, St. Martin said the problems are fixable and hopes speaking out will spark a conversation -- and change.
“I hope this resonates with enough people that we start a conversation and we start fixing the problem. It can be fixed,” he said.
“Let’s deal with the collegial part of ensuring the right person is transported to the right place at the right time, in a safe manner.”
CTVNews.ca Top Stories

The kids from 'Mrs. Doubtfire' are all SUPER grown up now, and we're not OK
The adorable trio of child actors from the 1993 classic comedy 'Mrs. Doubtfire,' which starred the late and great Robin Williams, are all grown up and looking back on their seminal time together.
Two killed after collision with truck on Hwy. 417 near Limoges, Ont.
Ontario Provincial Police say two people were killed after a car and a transport truck collided in the westbound lanes of Highway 417 near Limoges, Ont. on Tuesday afternoon.
‘We made them safer and more fun’: Here’s what’s new about e-scooters
Electric scooters (e-scooters) have been gaining popularity in the capital and this season comes with some changes and updates.
Houston braces for flooding to worsen in wake of storms
High waters flooded neighborhoods around Houston on Saturday following heavy rains that have already resulted in crews rescuing hundreds of people from homes, rooftops and roads engulfed in murky water.
A Chinese driver is praised for helping reduce casualties in a highway collapse that killed 48
A Chinese truck driver was praised in local media Saturday for parking his vehicle across a highway and preventing more cars from tumbling down a slope after a section of the road in the country's mountainous south collapsed and killed at least 48 people.
Canadian Auger-Aliassime reaches first Masters final in Madrid with another walkover
Montreal's Felix Auger-Aliassime has advanced to his first ATP Masters final, and he hasn't had to play all that much tennis to do it.
Drew Carey is never quitting 'The Price Is Right'
Drew Carey took over as host of 'The Price Is Right' and hopes he’s there for life. 'I'm not going anywhere,' he told 'Entertainment Tonight' of the job he took over from longtime host Bob Barker in 2007.
The UN warns Sudan's warring parties that Darfur risks starvation and death if aid isn't allowed in
The United Nations food agency warned Sudan's warring parties Friday that there is a serious risk of widespread starvation and death in Darfur and elsewhere in Sudan if they don't allow humanitarian aid into the vast western region.
Grandparents killed in wrong-way crash on Hwy. 401 identified
A 60-year-old man and a 55-year-old woman killed in a wrong-way crash on Highway 401 earlier this week have been identified by the Consulate General of India in Toronto.