Northern Ont. EMS wants to be first in Canada to offer opioid treatment in ambulances
Cochrane District EMS deputy chief Seamus Murphy watches as paramedics rush to a call at Timmins’ homeless shelter.
“My guess is it’s for an opioid overdose,” says Murphy, the deputy chief of standards and community services.
The current protocol is to give the patient naloxone to reverse the effects of an overdose and save the person’s life. Oftentimes, a bystander has already revived him or her with the medication.
Paramedics then offer to take the patient to the Timmins and District Hospital.
But Murphy says while this system has been saving lives —EMS responded to at least 200 opioid-related calls this year —there are still flaws.
For one, he says naloxone causes withdrawal symptoms to kick in as soon as it reverses the overdose. That can make patients irritable, aggressive and more likely to use again, should they refuse further treatment.
“Basically, we’ve taken away their high,” Murphy says.
“It kicks all of those opiates off of the opioid receptors and it keeps them safe for up to 90 minutes.”
That’s akin to quitting opioids ‘cold turkey,’ which brings on withdrawal symptoms like nausea, vomiting, diarrhea and anxiety.
And research shows that people who suddenly stop using opioids are up to 90 per cent more likely to use them again and have a higher likelihood of dying.
OPIOID THERAPY CAN SAVE LIVES
But if patients go to hospital, they’ll have access to opioid agonist therapy, which involves taking a long-acting opioid that can ease those symptoms and block the effects of other opioids.
Methadone is the most well-known therapy, but it requires a specialized facility and can take weeks to be fully effective.
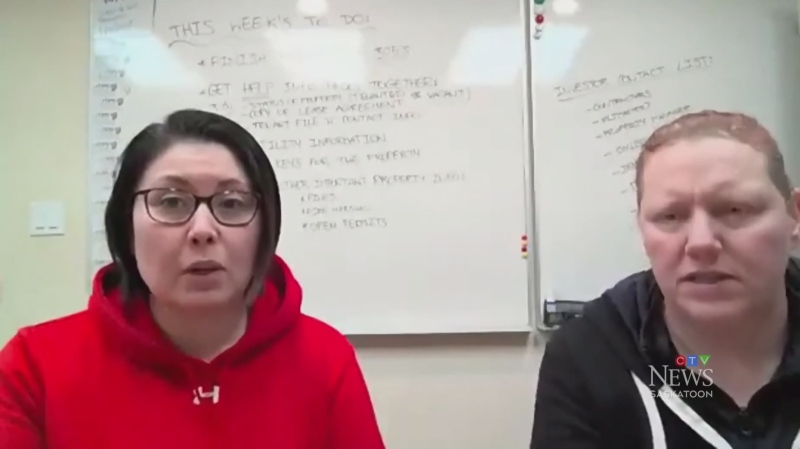
Instead, Drs. Louisa Marion-Bellemare and Julie Samson offer injections of buprenorphine. It takes full effect within 24 hours and protects patients from overdoses for about a month.
They also offer an even quicker-acting version in pill or film form.
“It treats their withdrawal symptoms within 30 minutes to an hour,” says Samson.
“Then, once it’s in their system and on those receptors in the brain, it prevents them from overdosing again.”
That form of buprenorphine—more commonly known by the brand Suboxone—protects patients for up to 36 hours. Like the injectable, it keeps stronger opioids from taking hold of the brain and allows the patient to function without feeling euphoric or sleepy.
Suboxone contains both buprenorphine and naloxone to combat opioid dependency and withdrawal.
The doctor duo says opioid agonist therapies reduce fatalities by 70 to 80 per cent. And that’s even if the patient continues using other opioids.
“It treats withdrawals, it treats cravings and it protects people from overdose and death, specifically to opiates,” says Marion-Bellemare.
FALLING THROUGH THE CRACKS
For those who decline transport to the hospital, the treatments are difficult to access.
Murphy says about 25 per cent of opioid overdose victims revived by EMS refuse further medical help. Those are people most likely to use again and potentially die.
While Cochrane District EMS (CDEMS) was the first in Ontario to carry naloxone in its ambulances, he says that’s no longer enough.
Now, he and the two doctors want paramedics to handle Suboxone themselves and offer the film version to patients on-scene.
“What we want to do is provide them something that will help them cope with their every day and give them time to get into a treatment program,” Murphy says.
The hope is that the drug therapy will get patients into a clearer state of mind and choose to continue on the path to sobriety through the regional hospital.
BETTER PATHWAY TO SOBRIETY
Murphy’s research shows 74 per cent of people who undergo opioid agonist therapies like buprenorphine stay in addictions treatment programs. He says patients are more likely to find a job, have stable housing and keep their families together.
But to make paramedics qualified to handle the drug, Ontario’s Ministry of Health needs to approve it.
Murphy presented his research and recommendations to the Ontario Base Hospital group, which manages paramedic health care in the province, to what he called overwhelming support.
The group will now be requesting that the ministry allow CDEMS to pilot the program.
FIRST PROGRAM OF ITS KIND IN CANADA
Marion-Bellemare and Samson got the idea from an EMS in New Jersey.
As far as they and Murphy can tell, no paramedic service in Canada is doing this right now. So if CDEMS takes it on, it would be the first program of its kind in the country.
“We will be ready to start, as soon as the ministry says go for it,” Murphy says.
The hope is to get approval to pilot the program in the New Year. He’s already training his paramedics on what buprenorphine is and how they would administer it in the field.
If all goes well, Murphy wants to roll the program out across Ontario and offer his insights to as many paramedic services that will hear him out.
“It’ll be a great feeling to see that we’re actually making a difference for these people,” Murphy says.
“We see them at their worst. We want to see them better.”
CTVNews.ca Top Stories

BREAKING Police to announce arrests in Toronto Pearson airport gold heist
Police say that arrests have been made in connection with a $20-million gold heist at Toronto Pearson International Airport one year ago.
LIVE @ 4 EDT Freeland to present 2024 federal budget, promising billions in new spending
Canadians will learn Tuesday the entirety of the federal Liberal government's new spending plans, and how they intend to pay for them, when Deputy Prime Minister and Finance Minister Chrystia Freeland tables the 2024 federal budget.
Proposed class-action lawsuit against Shoppers Drug Mart alleges 'unsafe and unethical corporate practices'
Shoppers Drug Mart is facing a proposed class-action lawsuit by current and former franchise owners at the retail chain who allege parent company Loblaw engaged in corporate practices that placed them in an “irredeemable conflict of interest” and put patient care at risk.
Lululemon unveils first summer kit for Canada's Olympic and Paralympic teams
Lululemon says it is combining function and fashion in its first-ever summer kit for Canada's Olympians and Paralympians.
Outdated cancer screening guidelines jeopardizing early detection, doctors say
A group of doctors say Canadian cancer screening guidelines set by a national task force are out-of-date and putting people at risk because their cancers aren't detected early enough.
Canada's health-care crisis was 'decades in the making,' says CMA
The strain placed on Canadian health care during the COVID-19 pandemic shows no sign of abating, and the top official of the Canadian Medical Association (CMA) is warning that improving the system will be a 'slow process' requiring sustained investment.
'I just started crying': Blue Jays player signs jersey for man in hospital
An Ontario woman says she never expected to be gifted a Blue Jays jersey for her ailing husband when she sat alone at the team’s home opener next to a couple of kind strangers.
Mussolini's wartime bunker opens to the public in Rome
After its last closure in 2021, it has now reopened for guided tours of the air raid shelter and the bunker. The complex now includes a multimedia exhibition about Rome during World War II, air raid systems for civilians, and the series of 51 Allied bombings that pummeled the city between July 1943 and May 1944.
B.C. woman facing steep medical bills, uncertain future after Thailand crash
The family of a Victoria, B.C., woman who was seriously injured in an accident in Thailand is pleading for help as medical bills pile up.